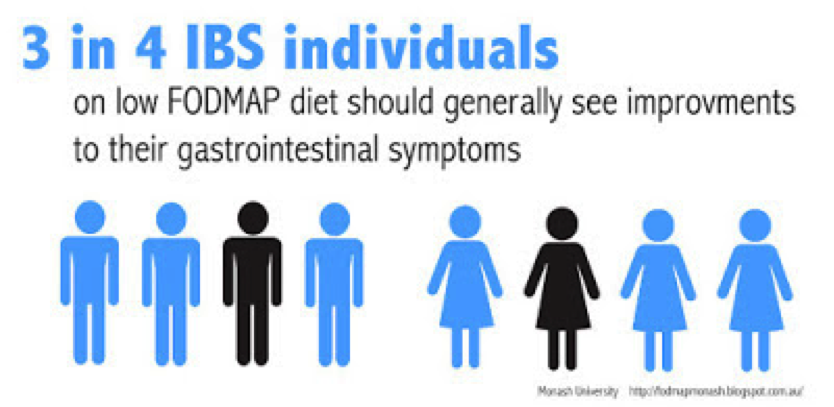
The low FODMAP diet has been shown to improve gastrointestinal symptoms in 3 out of 4 people with Irritable Bowel Syndrome (IBS), meaning a small percentage of people with this condition do not respond to the diet. So what should you do if you think you’re a ‘non-responder’?
Before dismissing the low FODMAP diet approach, it’s important firstly to ensure you’ve strictly adhered to the low FODMAP diet for at least 2 (and up to 6) weeks, ideally under the supervision of a dietitian specialised in using the diet. Use the app or booklet to double-check the FODMAP content of foods you’re eating and ask your dietitian to check your diet for hidden sources of FODMAPs. A specialist dietitian can also help to identify additional dietary triggers that may be aggravating your symptoms, such as caffeine, alcohol and/or spicy foods.
If you’re still experiencing no improvement in your symptoms, it might be worth returning to your Gastroenterologist for further investigations, or seeing a Dietitian who can investigate other dietary triggers, such as naturally occurring food chemicals (salicylates, amines and glutamates) that may be responsible for triggering IBS symptoms in a small proportion of people.
Aside from the low FODMAP diet, your Gastroenterologist or Dietitian may be able to advise you on the use of other therapies, including:
[1] Peters S, Yao CK, Shepard S, Philpott H, Yelland G, Muir J.G., Gibson P.R. Su1369 Gut-Directed Hypnotherapy and a Low FODMAP Diet Are Similarly Efficacious in Patients With Irritable Bowel Syndrome: A Randomised Controlled Non-Inferiority Trial. Gastroenterology 2015: 148(4) Supp 1, 487-488
[2] Tuck CJ, Muir JG, Barrett JS, Gibson PR. Fermentable oligosaccharides, disaccharides, monosaccharides and polyols: role in irritable bowel syndrome. Exp Rev Gastroenterol Hepatol 2014:1-16.
[3] Khanna, R, MacDonald, J.K, Levesque, B.G. (2014). Peppermint oil for the treatment of irritable bowel syndrome: a systematic review and meta-analysis. J Clin Gastroenterol, 48(6):505-12