
Endometriosis is a gynaecological condition characterised by the presence of endometrial-like tissue outside the uterus (1). Endometriosis affects 1 in 7 Australian women aged up to 49 years (2) and has a profound negative impact on quality of life (1). While characteristic symptoms include dysmenorrhoea (painful periods), pelvic pain (pain in the lower abdomen and above the legs), dyspareunia (painful sexual intercourse) and dysuria (painful urination), gastrointestinal (GI) symptoms such as abdominal pain, bloating, diarrhoea and dyschezia (painful defecation) are extremely common, affecting > 75% of individuals (3-5).
Frustratingly for sufferers however, few endometriosis treatments specifically target GI symptoms, and some (such as opioid medications and progesterone) can make these GI symptoms worse (4). Furthermore, most treatment guidelines also fail to mention the GI symptoms associated with endometriosis, leaving clinicians little guidance on best practice management (5, 6).
We know from research and clinical practice that many women with endometriosis will alter their diet in an attempt to manage their symptoms, but until now there was very limited evidence to suggest that any particular dietary approach was effective.
Given the overlapping GI symptoms between IBS and endometriosis and some preliminary data suggesting a benefit of FODMAP restriction for GI symptoms related to endometriosis (7), we set out to test the effectiveness of a low FODMAP diet in a single blinded, randomised controlled, crossover feeding study. Thirty-five women with endometriosis and poorly controlled GI symptoms were enrolled into the study. The women were randomised to 1 of 2 different diets, both of which were nutritionally matched and modelled on Australian Dietary Guidelines, but only 1 of which was low in FODMAPs. Most food was supplied to participants in this feeding study, and participants were instructed to consume the supplied diet for 28 days, before washing out for 28 days and crossing over to the alternate dietary intervention.

Our study showed that 60% of participants responded to the low FODMAP diet, and experienced clinically significant improvements in their GI symptoms, compared to 26% that responded to the control diet. Improvements were also seen in abdominal pain, bloating, and quality of life. Gastrointestinal symptoms continued to improve over the 4 weeks on the low FODMAP diet, with meaningful improvements seen after 2 weeks.


The findings are exciting news for women with endometriosis, providing an effective, evidence-based diet therapy, when previously there was none. Given how prevalent endometriosis is, and that the majority of sufferers report troublesome GI symptoms, this diet has the potential to positively impact the lives of many women.
Further research is needed to evaluate the benefits of this diet in a larger population and over the longer term. This was also a proof-of-concept feeding study, whereby all food was supplied to participants. We would like to evaluate the real-world effects, by having dietitians teach the diet and patients to implement the diet using this advice.
Patients seeking further information should talk to a dietitian trained in delivering a FODMAP diet or head to monashfodmap.com to find a range of resources such as the Monash FODMAP diet App and online courses, all designed to support patients and clinicians to implement a low FODMAP diet.
Read the full research publication here.
We have also created a handy new endometriosis-specific 3-step diet flyer!
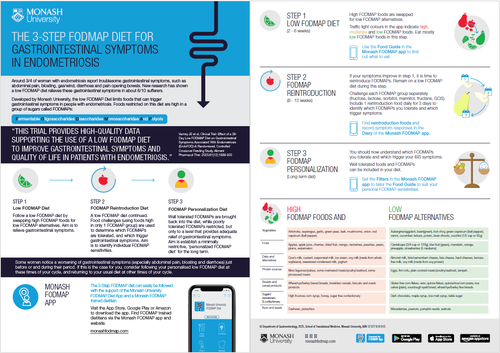
You can download the PDF here:
References